Introduction:Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing novel COVID-19 is spreading all across the globe like wildfire. As was the case with severe acute respiratory syndrome coronavirus (SARS) in 2002 and Middle East respiratory syndrome (MERS) in 2012, several hematological laboratory abnormalities have been identified. Several studies have reported prevalence and mechanism behind COVID-19 patients presenting with thrombocytopenia, however its association with disease severity and mortality is poorly understood. In this study we seek to investigate these clinical outcomes.
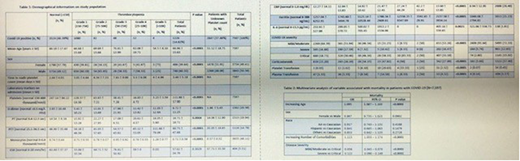
Methods:Retrospective data on 7597 consecutive hospitalized patients with COVID-19 was recorded. Data included demographical information, comorbidities, admission laboratory markers, nadir platelet count and time to platelet nadir. Platelet count was categorized as grade 1 (150K-75,001), grade 2 (75K-50,001), grade 3 (50K-25,001), grade 4 (25K-10,001), and grade 5 (<10K). COVID-19 disease severity was defined as mild/moderate (medical floor), severe (ICU), and critical (ICU and ventilator/vasopressor use). In-hospital mortality was also analyzed.
Results:Of the 7,597 confirmed COVID-19 patients, 1,226 (16%) patients had some degree of thrombocytopenia (platelet count <150K/mm3), while 3524 (46%) did not. No platelet count was available for 2,847 (38%) patients. In patient population with thrombocytopenia, mean age was 67 years and included 486 (40%) female. Variables that had an association with degree of thrombocytopenia with statistical significance included increasing mean age, male sex, increased time to nadir platelet count, and elevated laboratory markers on admission (d-dimer, prothrombin time (PT), partial thromboplastin time (PTT), monocytes, c-reactive protein (CRP), ferritin, interleukin-6 (IL-6)). Degree of thrombocytopenia also was associated with increasing COVID-19 disease severity (table 1). Overall, 1,163 (15%) of patients died in hospital or were discharged to hospice care. In multivariate analysis, patients with grade 1 thrombocytopenia were 1.448 times more likely to die that those patients with no thrombocytopenia when controlling for the other variables (p value =0.0004). Similarly, grade 2 were 3.916 times more likely to die (p value <0.0001), grade 3 were 7.736 times more likely to die (p value <0.0001), grade 4 were 34.346 times more likely to die (p value =0.0014), and grade 5 were 108.925 times more likely to die (p value =0.0011). Interestingly, interventions such as steroids use was associated 1.43 times increase in mortality (p value =0.0002), while plasma transfusion was associated with 2.43 times increase in mortality (p value =0.0018) (table 2).
Conclusion:Thrombocytopenia is common among patient with COVID-19. We report prevalence of thrombocytopenia in COVID-19 patients to be comparable to other studies (16%). COVID-19 patients with thrombocytopenia were noted to be older compared to patients without thrombocytopenia (67 vs 60 years). As a result, this population may have other comorbidities that make them more vulnerable and susceptible to hematological abnormalities. As expected, most patients were categorized as grade 1 thrombocytopenia (88%) and very few patients had indication for platelet transfusion (grade 5 thrombocytopenia <1 %). Several concurrent abnormal inflammatory laboratory markers point towards consumptive thrombocytopenia in the setting of hyper-inflammatory phase COVID-19. This is consistent with time to nadir platelet count seen in this study- day 3 to 8 with increase in degree of thrombocytopenia. More importantly, we see that thrombocytopenia is associated with increases in disease severity and mortality. The higher the degree of thrombocytopenia the more likely the patient may require ICU level of care and mechanical ventilator support. Overall, we see that COVID-19 patients with thrombocytopenia exhibit worse outcome in terms of disease severity and mortality when compared to patients without thrombocytopenia. The etiology behind this association is still unclear and presents an area for future research.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal